Can Sleep Apnea Contributes to Hair Loss?
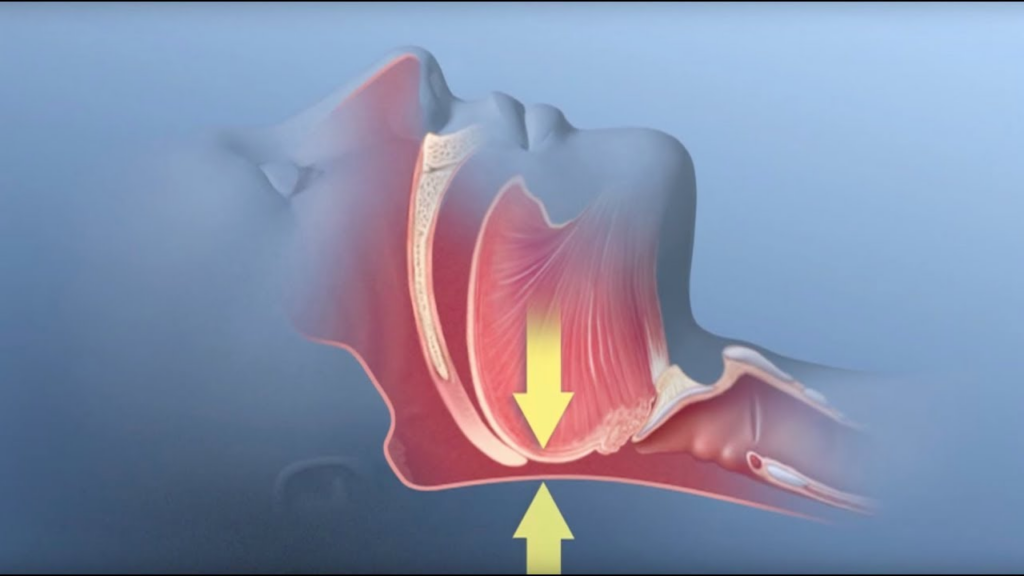
People with sleep apnea feel exhausted the next day, even after getting a “full” night’s rest. The very idea of having blocked or lapsed breathing is frightening enough, but those who really have it also suffer from secondary concerns including marital troubles, weight gain, and reduced cognitive functioning. These problems are caused by the secondary …